House Calls Helping Vulnerable Seniors Age at Home Through the COVID Crisis

The isolation, physical distancing, stockpiling and stay-at-home orders that we have all navigated over the past few months are not a new reality for the marginalized, home-bound seniors that the House Calls program has supported for over twelve years. Seniors with medical, cognitive and social frailty are particularly vulnerable to COVID-19 and House Calls has continued to help their patients stay out of hospital, out of long-term care and safe in their own homes.
House Calls began as a pilot project in 2007 by Dr. Mark Nowaczynski, a Toronto-based family physician, after witnessing the lack of in-home primary care for elderly patients with complex, chronic disease who wanted to age in place. Dr. Nowaczynski, a skilled photographer, used black and white documentary photography to bring attention to the challenges and needs of this growing and under-served population that he saw as falling through the cracks of our health care system. Through this advocacy and education—with SPRINT Senior Care as the Lead Administrative Agency—House Calls built collaborations with other not-for-profit organizations including VHA Home HealthCare (VHA), formed a unique partnership with the Department of Geriatrics at Mount Sinai Hospital and secured additional funding through the Ontario Ministry of Health and Long-Term Care.
VHA Home HealthCare became involved in 2008 by donating human resource support to this initiative and VHA’s own Leslie Coulter was the first occupational therapist (OT) brought on board. “After fighting for dollars and a lot of advocacy work, our program has now grown to 17 health professionals—seven family doctors, two nurse practitioners, three occupational therapists, a physiotherapist, two social workers and two team coordinators—with a catchment area that reaches almost half the city of Toronto and serves close to 1,000 patients every year,” said Leslie. “House Calls replaces an office-based primary-care provider with a mobile, interprofessional team to provide ongoing care for frail, vulnerable seniors whose needs are not being met by the traditional health care system. Homebound patients tend to not advocate for themselves and can be invisible if we’re not looking—providing this service for them is a necessity and not a convenience,” she said.
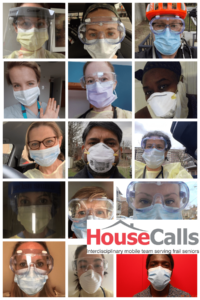
From top left to right: Natalie Leventhal (SPRINT Senior Care), Dr. Christa Sinclair-Mills, Dr. Mark Nowaczynski, Dr. Elizabeth Niedra, DeeDee McEwan (VHA Home HealthCare), Teresa Sparks (SPRINT Senior Care), Stacey Pustowka (SPRINT Senior Care), Parag Agarwal (VHA Home HealthCare) , Dr. Katja Heineck, Dr. Shayna Singh, Gayle Cronin (VHA Home HealthCare), Leslie Coulter (VHA Home HealthCare), Sherri Dakin (VHA Home HealthCare), Lindsay Jones (VHA Home HealthCare), Alain Fon (SPRINT Senior Care)
As COVID-19 started to spread across the province, Leslie and her House Calls team were very concerned about how inevitable service interruptions would impact an already vulnerable population. “In the home care world, we are very used to barriers to care but COVID-19 introduced brand new ones. We had to move quickly and adapt faster—without a lot of guidelines for home-based interdisciplinary care—to keep our patients out of hospital and in their homes, while ensuring everyone’s safety,” said Leslie. “It was like a spark was lit underneath us. The perseverance, flexibility, positivity and collaboration I’ve witnessed around me over the last few months has been unparalleled,” she said.
The team had the difficult task of identifying who out of their high-need patient population were the most vulnerable, who would continue to have in-person visits and how to effectively use virtual care when in-person visits were deemed unnecessary or too high-risk. “We prioritized visits that would reduce hospitalizations and complications and where there was functional decline, end-of-life care, food insecurity or urgent mobility or home safety concerns,” said Leslie.
Phone calls have been helpful for follow-up, triage, joint-visits with other specialists and to minimize the time spent in patients’ homes, but that is only a band-aid option during a time of crisis. “At an average age of 88, with sensory impairments, limited access to technology and generally no family or caregiver support, for our patients phone calls are the only way to connect virtually and there are a lot of limitations to telephone care,” said Leslie.
Leslie and her team have navigated many challenges including donning and doffing of personal protective equipment (PPE) safely in the community, connecting with and communicating to patients with cognitive or hearing impairments in full PPE, no access to bathrooms, no office space for charting, and of course, the crippling fear of getting a vulnerable patient sick, or bringing the virus back to their own families. “But what we’re most proud of is that this pandemic hasn’t left our patient population without care. We had the same number of patient encounters at this time in 2020 as we did in 2019, and that’s so reassuring,” said Leslie. “There’s an opportunity for some really impactful research on how this program prevented hospitalizations and institutionalizations once we are able to slow down, catch our breath and conduct some research,” she said.
COVID-19 has revealed more than ever that long-term care facilities aren’t always the best way to care for our seniors. “Home-based primary care is an under-appreciated and minimally-supported part of our health care system. If you have physicians willing to do house calls and can wrap an interprofessional team around them, in many cases, it’s safer and less costly for seniors that want to stay in their homes. We believe that this program can be replicated and expanded, we just need the engagement and funding to support this,” said Leslie.
To learn more about the House Calls program, visit seniorshousecalls.ca and watch the powerful National Film Board award-winning documentary House Calls.
